Definition
- An artery dilatation >50% (X1.5) of its original diameter is called aneurysm
- True aneurysm: dilatation of all layers of the blood vessels
- False aneurysm (pseudoaneurysm): dilatation of aventitia which communicated with lumen usually following trauma
- Types of aneurysms are listed
- Berry aneurysm- bulges from one side of the artery
- Fusiform aneurysm- bulges from all sides of an artery
- Giant aneurysm- involve more than one artery. It is over 2.5 cm wide
- Mycotic aneurysm- caused by infected artery wall
Risk factors
- Male
- Over 65 years of age
- Atherosclerotic factors: hypertension, smoking, obesity, sedentary lifestyle, hyperlipidaemia, diabetes
- Family history of AAA: 10% risk if first-degree relative affected
- Congenital - berry aneurysms
- Infective - mycotic aneurysms
- Traumatic - non/penetrative
- Inflammatory - vasculitis
- Connective tissue disorders- Marfan’s Syndrome and Ehlers-Danlos Syndrome
- Cocaine - can cause aortic, cerebral and peripheral aneurysms
REMEMBER: 1 in 25 males over 65, without having additional risk factors, will be found to have an AAA. However, 1 in 6 males with accompanying risks factors, will have an AAA.
Examination
- Normal abdominal aorta will be pulsatile not expansile
- AAA will be pulsatile and expansile
- Expansile abdominal mass (it expands and contracts)
- Swelling that are just pulsatile
- Shock (in rupture)
Genetic component involved so there is familial cluster. Ask specifically for family Hx of AAA or other aneurysm
Common sites of AAA
- Aortic (infra-renal accounts for 90% of cases) [1]
- Iliac
- Popliteal (accounts of 80% of all peripheral aneurysm, usually bilateral)
- Femoral (can be felt as lump in the groin)
- Thoracic aneurysms (accounts for 10% of cases)
Presentation
- Unruptured AAA
- Often none
- May cause abdominal/back pain
- Often discovered incidentally in US or CT KUB
- Ruptured AAA
- Intermittent/ continuous abdominal pain (with radiation to back or groin)
- Collapse
- Hypovolaemic Shock
Differential diagnosis
- Renal colic
- Acute pancreatitis
- Diverticulitis
- Testicular pain
- Erosion of vertebral bodies
NEVER miss AAA in someone complaining of loin to groin pain.
Complications of AAA
- Rupture (increases with age for individuals >65yrs)
- Thrombosis/embolism
- Blood often slow around the edges of aneurysm sac leading to thrombus formation and emboli occluding peripheral arteries è pt can present with limb ischaemia/claudication
- Fistulae
- Pressure on surrounding structure
Investigations
- Imaging
- US for monitoring
- CT for anatomical details, to look for ‘crescent sign’- sign of impending rupture
- Other
- FBC, clotting factor, renal and liver function, and cross match for surgery
Management
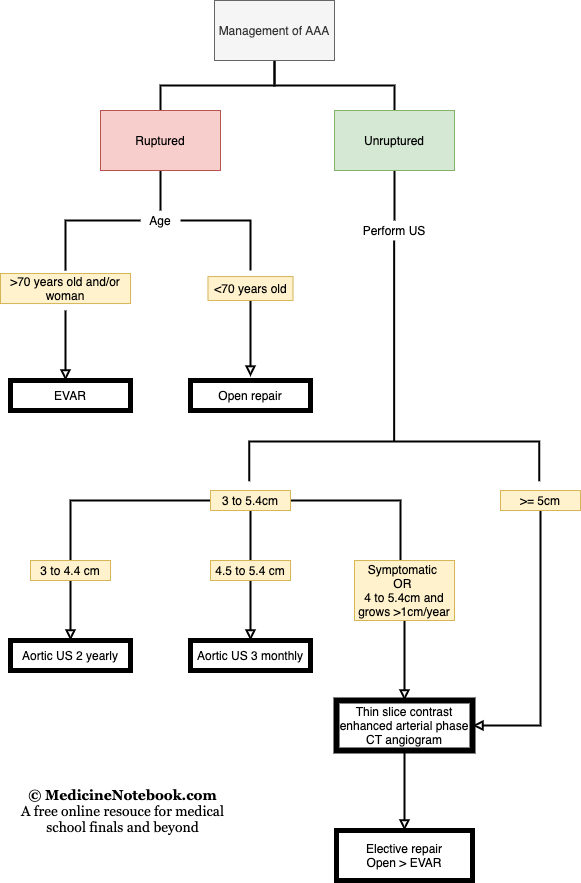
- Ruptured aneuryms
- Repair either by EVAR or Open surgery
- Unruptured aneurysm
- Repair if;
- symptomatic
- asymptomatic, larger than 4.0 cm and has grown by more than 1 cm in 1 year
- asymptomatic and 5.5 cm or larger
- Repair if;
-
The relevant provisions of § 2323 allow for the forfeiture of “(A) Any article, the making or trafficking of which is, prohibited under section 506 of title 17″ prohibiting “willful copyright infringement” and “(B) Any property used, or intended to be used, in any manner or part to commit or facilitate the commission of an offense referred to in subparagraph (A) ↩