urology,
Testicular cancer
May 10, 2020
Epidemiology
- Most common malignancy in males aged 15-44 yo
- 10% occur in undescended testes, even after orchidopexy
Risk factors:
- Cryptorchidism
- infertility
- family history
- Klinefelter’s syndrome
- mumps orchitis
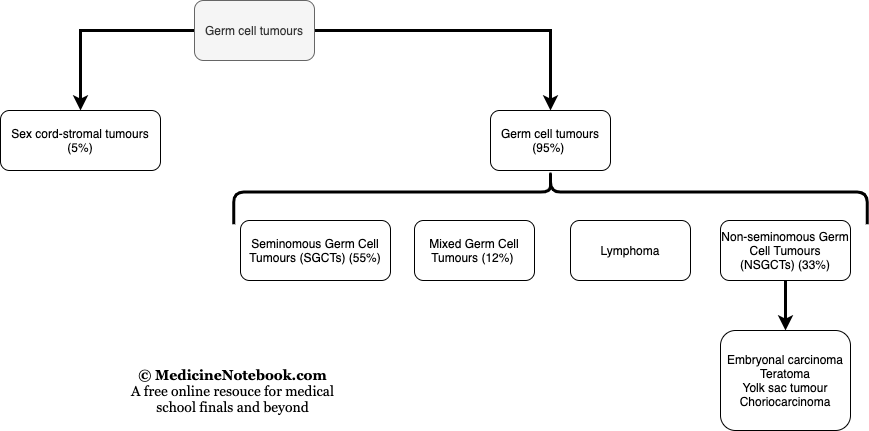
Classification
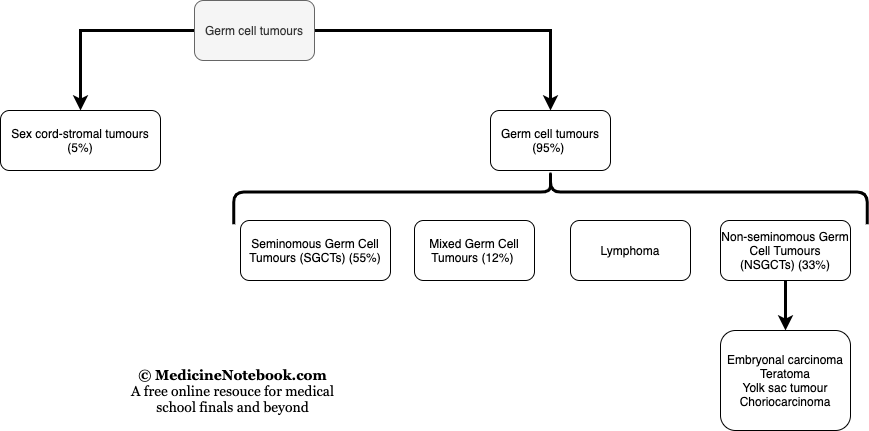
Classification of Testicular tumour
Presentation:
- Usually painless lump
- Painful lump if bleeds inside or infection
- Rarely, changes in testicular volume or consistency
- Longer history in seminoma pt than non-seminoma
- Signs of metastasis
- supraclavicular lymph node
- Dyspnoea from pulmonary mets
Investigations:
- Bloods: AFP, B-hCG, Lactate dehydrogenase
- Imaging
- 1st line: Ultrasound colour Doppler
- Other: CT abdomen and chest for staging
Seminomous Germ cell tumour
- Older patients (avg. 40 years)
- 25% metastasise at presentation
- Excellent prognosis even with advanced disease (5 year survival of 73%)
- Tumour marker not typically raise: AFP normal, ↑ HCG (10%), ↑LDH (10%)
- Strong association with cryptorchidism
- May present with mass in the undescended testes in the inguinal region or the abdomen
Non-seminomatous germ cell tumours
- Younger patients (20-30 year olds)
- Advanced disease = poor prognosis (48% at 5 years)
- Biomarkers
- Embryonal carcinoma: ↑AFP /↑B-hCG
- Yolk sac tumour: ↑AFP characteristic
- Choriocarcinoma:↑B-hCG characteristic
- Teratoma: ↑AFP /↑B-hCG
Sex cord-stromal tumour
- Arise from supportive connective tissue around germ cells
- Rare, less than 5% of testicular cancer
- Excellent prognosis after surgical resection
- Two types of tumour: Leydig cell tumour, Sertoli cell tumour
Lymphoma
- Most common cause of a testicular mass in males > 60 years old; often bilateral
- Usually of diffuse large B-cell type
Staging
- Stage 1: No evidence of metastasis
- Stage 2: Infradiaphragmatic node involvement (spread via para-aortic nodes)
- Stage 3: Supradiaphragmatic node involvement
- Stage 4: Lung involvement (haematogenous)
Management
- SGCT
- Orchidectomy (via inguinal approach to prevent lymphatic spread)
- Extremely radiosensitive
- NOTE: orchidectomy and radiotherapy cures 95% in stage 1
- NSGCT
- Orchidectomy (inguinal approach)
- 3 cycles of Bleomycin + Etoposide + Cisplatin
- Follow-up
- Do close follow up using biomarkers, reviews and self-examination