Pathology
- Mostly adenocarcinomas
- Arises on the peripheral zone of the prostate
- Mostly slow-growing but some can be aggressive
- Commonly metastesise to lymph nodes and bones
Epidemiology
- The most common cancer in men
- Its incidence increases with age: 20% in 50s and 70% in 70s
- Subclinical prostate cancer is common in men aged over 50 years
Risk factors
- Advanced age
- Afro-Caribbean mean (increased incidence and mortality)
- If one first-degree relative has prostate cancer, the risk is doubled
- Food consumpution (high intake of animal fat and lower intake of fruits, cereals and vegetables)
- Alcohol consumption
- Pattern of sexual behaviour
- Chronic inflammation and occupational exposure
Screening
- No screening in the UK
- UK Rational: only small reduction in mortality but ↑ diagnostic and treatment harms
Presentation
- Local disease:
- Raised PSA
- LUTS
- Urinary tract infection.
- Locally invasive disease:
- Haematuria, dysuria, incontinence.
- Haematospermia (blood in ejaculation)
- Perineal and suprapubic pain.
- Obstruction of ureters, causing loin pain, anuria, symptoms of acute kidney injury or chronic kidney disease.
- Rectal symptoms - eg, tenesmus (recurrent inclination to empty bowel)
- Metastatic disease (think about metastasis to bones and lymph nodes):
- Bone pain or sciatica.
- Paraplegia secondary to spinal cord compression.
- Lymph node enlargement.
- Loin pain or anuria due to ureteric obstruction by lymph nodes.
- Lethargy (anaemia, uraemia).
- Weight loss, cachexia.
Signs
- Look for red-flag symptoms in advanced disease:
- General malaise
- Bone pain (due to metastasis)
- Anorexia
- Weight loss
- Obstructive nephropathy
- Paralysis due to cord compression (secondary to metastasis)
- Distended bladder due to overflow obstruction
- DRE examination may reveal a hard, irregular prostate gland. Indication of possible prostate cancer are:
- Asymmetry of the gland.
- A nodule within one lobe.
- Induration of part or all of the prostate.
- Immobile - adhesion to surrounding tissue
- Palpable seminal vesicles.
Differential diagnosis
- Benign prostatic hyperplasia (BPH)
- Any other cause of haematuria (e.g. UTI)
- Prostatitis
- Bladder tumour
Investigations
- PSA ↑
- Urinalysis: haematuria
- Renal function test to exclude renal pathology
- Trans-Rectal Ultrasound guided (TRUS) biopsy
- Transperineal template biopsy: if TRUS negative/ inconclusive but high suspicion
- MRI for staging
- Isotope bone scan for bone mets
Grading system
- Spread and staging by TNM scoring
- Aggressiveness assessed Gleason score
- Two areas of tumour specimen analysed for tumour differentiation: Well differentiated (scores 1) → Moderately differentiated → Poorly differentiated (scores 5)
- The worse score from added up to give 2-10
- 2-4= Indolent, 5-7= Intermediate, 8-10= Aggressive
Prognostic factors
Helps to determine between ‘watchful waiting’ vs aggressive treatment:
- Pre-treatment PSA level
- TNM staging
- Tumour grading- Gleason score
Risk stratification (NICE 2014):
Urology MDT should risk stratify localised disease (T1-T2) as follows:
- Low risk: PSA <10 and Gleason ≤6 and Stage T1 -T2a
- Intermediate risk: PSA 10-20 or Gleason 7 or T2b
- High risk: PSA >20 or Gleason 8-10 or ≥T2c
Management
Overview
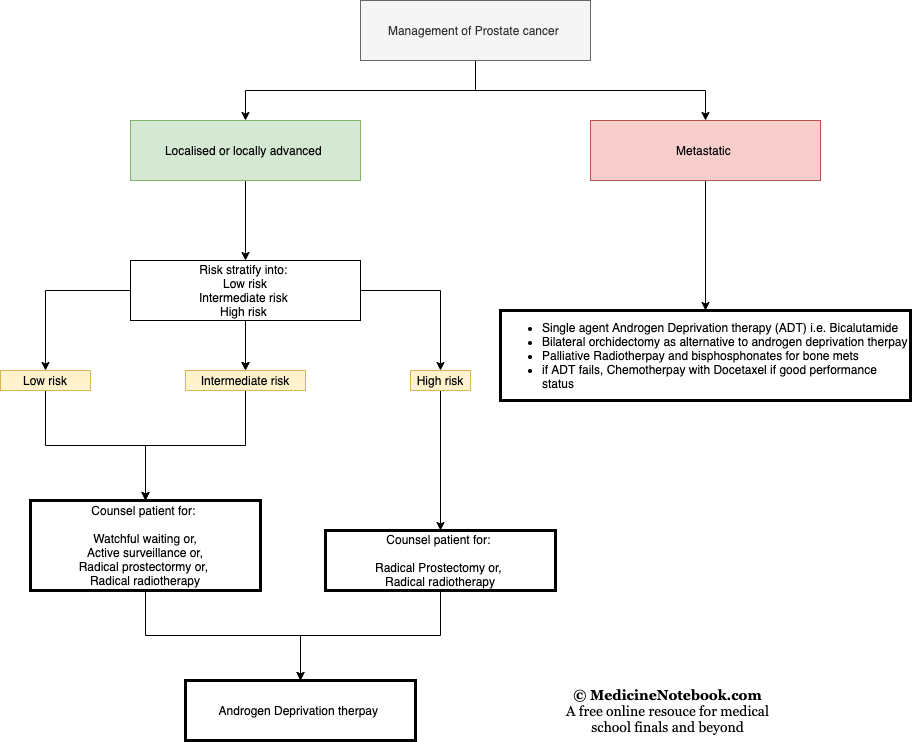
Conservative
- Watch and wait
- Indicated in elderly, multiple co-morbidities, low Gleason score with localised disease (harm from treatment > harm from cancer)
Surgical management
- Radical prostatectomy (open or laparoscopic)
- Generally recommended if life expectancy >10 years (usually offered to patients <70yrs)
- Robotic surgery
- SE: Erectile dysfunction (40-30%), Incontinence
Medical management
- Active surveillance
- Aimed at keeping patient within ‘window of curability’
- Part of curative strategy
- Delays radical treatment
- Finasteride
- Inhibitor of 5 alpha-reductase, an enzyme which metabolises testosterone into dihydrotestosterone. Used for LUTS
- SE: impotence, low libido, ejaculation disorders, gynaecomastia
- Radiotherapy
- External beam radiotherapy – along with surgery, this can be curative. More suitable in elderly but many younger and generally fit patient may chose it as an alternative to surgery. Adverse effects: proctitis, and rectal cancer
- Brachytherapy – radioactive ‘seeds’ are planted in the prostate by TRUS (Systemic SEs reduced) There are two types: Temporary high dose seeds (for advanced cancer) and Permanent low dose seeds (for early cancer)
- Androgen suppression
- Main treatment for metastatic disease
- Used intermittently in localised or locally advanced disease (to delay refractory disease)
- Response takes 24-36 months to develop but refractory disease eventually occur.
- Synthetic GnRH agonist e.g. Goserelin, Degarelix– these stop the release of lutenising hormone, and thus the production of testosterone. It first simulate and then inhibit pituitary gonadotrophin → so patient may develop flare-up → give caution → Use anti-androgen in adjunct in susceptible pts
- SEs: Hot flushes, Sexual dysfunction, Osteoporesis, Gynaecomastia, fatigue
- Anti-androgen drugs: Cyproterone Acetate
- Castration – unacceptable for many